What are the treatments for neuropathic pain?
We understand that neuropathic pain can be very debilitating, have a sudden onset and often stop you in your track. However, your prescribing doctor and treating pharmacist should have discussed with you that the medicines might only partly alleviate the symptoms. A pain management plan will look at other things you can do, along with taking your medicine, to help manage your pain.
Your treatment might include drug and non-drug options such as physiotherapy to help strengthen your muscles or if your neuropathy is caused by a pre-existing condition such as diabetes then you may benefit from an intervention such as a diabetes management review.
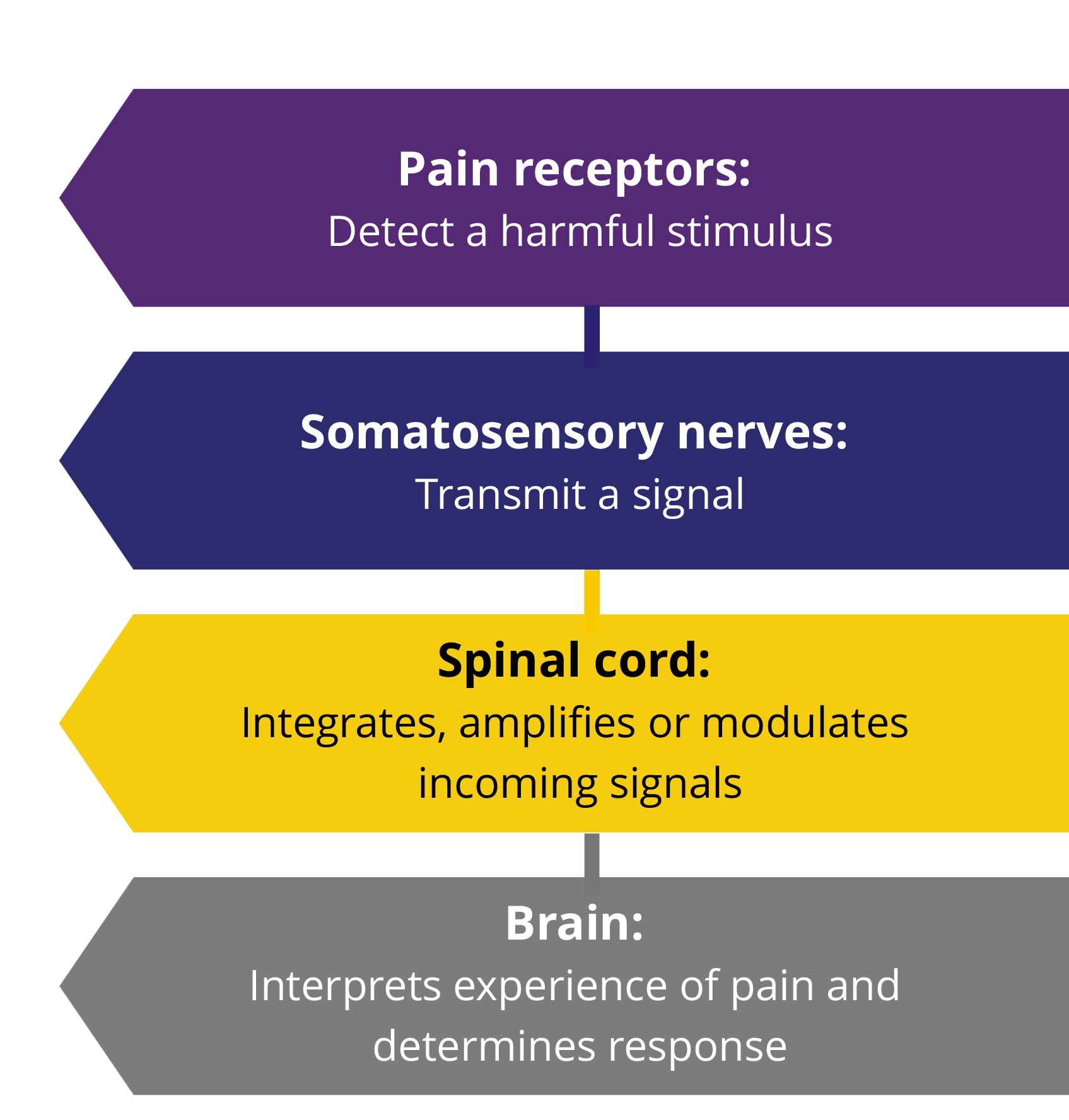
Neuropathic pain is not like other forms of pain, such as a pulled muscle or strain in which common pain killers like paracetamol such as paracetamol and/or ibuprofen can help. The medicines which are prescribed for neuropathic pain are different and can take longer to work.
When you start treatment with medicines for your neuropathic pain you may begin on a low dose, which your doctor may choose to increase over time, gradually, until you gain the most benefit. Some people find that they do not wish to increase the dose as they may experience side effects on a higher dose.
The most common side effects of medicines to treat neuropathic pain are tiredness, dizziness or feeling ‘drunk’. If you are experiencing these side effects, please have a discussion with your doctor. Do not drive or operate machinery if you experience drowsiness or blurred vision and follow advise by the doctor or pharmacist, also avoid alcohol.
Everyone is different and responds differently to drug treatment – some people find that their medicine starts to help straight away, and for others it takes a bit more time. It is important to keep talking to your doctor and /or pharmacist about how you are feeling, whether things are improving, and what you can do to help yourself.
If your symptoms worsen at any point please ensure you contact your prescribing doctor.